Planning for the future has been a primary focus of our Board of Directors
since 2012 and continues to be an objective in our Strategic Plan. This long-term
development plan for our facilities is imperative for us to ensure a
sustainable future for our hospitals in Bracebridge and Huntsville.
There are several reasons why we need new hospitals in Bracebridge and Huntsville. Our buildings from 1964 (SMMH) and 1978 (HDMH) today present many challenges that limit us. They are old buildings that do not meet current best practices and health care standards, including rules around privacy and infection control. Single occupant private rooms are not a nice to have, they are a need to have. Across both sites, only 15% of our rooms house a single patient with the majority as two-bed and four-bed rooms. Our buildings are also very difficult to adapt to advancing technologies within their existing footprints. We don’t have enough space for the care we deliver today, let alone the care our community will require in the future. On top of that, it is so important that our care providers have a work environment where they are equipped with the tools and the space to do their job of providing you with excellent care.
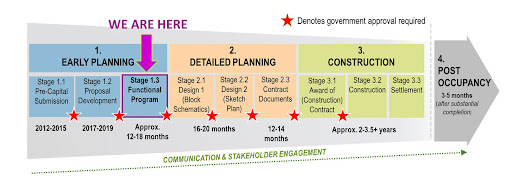
Following years of progress through the Ministry of Health’s capital planning process for hospitals, in April 2022 the Ontario government gave us the green light to move to the next stage of our planning for a new hospital on the existing land in Huntsville, and a new hospital at a new location in Bracebridge. Premier Doug Ford’s announcement was a significant milestone in our future planning journey and included grant money for the planning to continue (not for new construction). Over the next 12 to 18 months, we are working through what the Ministry refers to as the ‘Functional Program’ or Stage 1.3 of their planning process.
This stage involves detailed program and service planning to meet our community’s future needs, resulting in architectural drawings of the buildings and physical space needed to support the programs and services in new, state-of-the-art facilities. Everything we have learned from the pandemic will be considered, and the initial planning assumptions identified through earlier planning work are revisited to reflect the most current information on how people receive care locally through various health services and regionally through more specialized health centres. We are excited to embark on this work with expert consultants, supported by the in-depth knowledge of our staff and clinicians through internal focus groups. Patients and families from our communities will also be key to this work and will be involved at all levels of this project.
Another big component of this stage will be to get a clearer understanding of the cost of the future builds. The Ministry of Health pays for a portion of our project for two new hospitals, and the local community is expected to pay a “local share” of the entire project, which can be up to 30% of the total project cost, including furnishings, fixtures and hospital equipment. Our initial cost estimates will be updated to be more current to today’s economy and will also factor in the various cost inflation impacts of the COVID-19 pandemic. In our last planning submission to the Ministry in 2019, the local share was estimated at $129 million in 2019 dollars. New projections will try to forecast the potential cost by the time we are at the stage of building the two new hospitals, which may not start for seven or eight more years.
I am excited to provide this update on our redevelopment project and the work that we are undertaking over the next year or more. We are so grateful to our two hospital foundations and all of the local municipalities for their continued support and collaboration in determining the best path forward in how our communities will fund the local share. Working together will ensure this very important project for future hospital care in Muskoka continues to move forward.

.jpg)




